Will Posterior Tibial Tendon Dysfunction Require Surgical Teatments ?
Overview There are four stages of posterior tibial tendon dysfunction. In the first stage the posterior tibial tendon is inflamed but has normal strength. There is little to no change in the arch of the foot. In stage two the tendon is partially torn or shows degenerative changes and as a result loses strength. There is considerable flattening of the arch without arthritic changes in the foot. Stage three results when the posterior tibial tendon is torn and not functioning. As a result the arch is completely collapsed with arthritic changes in the foot. Stage four is identical to stage three except that the ankle joint also becomes arthritic.  Causes Damage to the posterior tendon from overuse is the most common cause for adult acquired flatfoot. Running, walking, hiking, and climbing stairs are activities that add stress to this tendon, and this overuse can lead to damage. Obesity, previous ankle surgery or trauma, diabetes (Charcot foot), and rheumatoid arthritis are other common risk factors. Symptoms Patients often experience pain and/or deformity at the ankle or hindfoot. When the posterior tibial tendon does not work properly, a number of changes can occur to the foot and ankle. In the earlier stages, symptoms often include pain and tenderness along the posterior tibial tendon behind the inside of the ankle. As the tendon progressively fails, deformity of the foot and ankle may occur. This deformity can include progressive flattening of the arch, shifting of the heel so that it no longer is aligned underneath the rest of the leg, rotation and deformity of the forefoot, tightening of the heel cord, development of arthritis, and deformity of the ankle joint. At certain stages of this disorder, pain may shift from the inside to the outside aspect of the ankle as the heel shifts outward and structures are pinched laterally. Diagnosis Perform a structural assessment of the foot and ankle. Check the ankle for alignment and position. When it comes to patients with severe PTTD, the deltoid has failed, causing an instability of the ankle and possible valgus of the ankle. This is a rare and difficult problem to address. However, if one misses it, it can lead to dire consequences and potential surgical failure. Check the heel alignment and position of the heel both loaded and during varus/valgus stress. Compare range of motion of the heel to the normal contralateral limb. Check alignment of the midtarsal joint for collapse and lateral deviation. Noting the level of lateral deviation in comparison to the contralateral limb is critical for surgical planning. Check midfoot alignment of the naviculocuneiform joints and metatarsocuneiform joints both for sag and hypermobility. Non surgical Treatment Flatfoot deformity can be treated conservatively or with surgical intervention depending on the severity of the condition. When people notice their arches flattening, they should immediately avoid non-supportive shoes such as flip-flops, sandals or thin-soled tennis shoes. Theses shoes will only worsen the flatfoot deformity and exacerbate arch pain. Next, custom orthotics are essential for people with collapsed arches. Over-the-counter insoles only provide cushion and padding to the arch, whereas custom orthotics are fabricated to specifically fit the patient?s foot and provide support in the arch where the posterior tibial tendon is unable to anymore. Use of custom orthotics in the early phases of flatfoot or PTTD can prevent worsening of symptoms and prevent further attenuation or injury to the posterior tibial tendon. In more severe cases of flatfoot deformity an ankle foot orthosis (AFO) such as a Ritchie brace is needed. This brace provides more support to the arch and hindfoot rather than an orthotic but can be bulky in normal shoegear. Additional treatment along with use of custom orthotics is use of non-steroidal anti-inflammatories (NSAIDS) such as Advil, Motrin, or Ibuprofen which can decrease inflammation to the posterior tibial tendon. If pain is severe, the patient may need to be placed in a below the knee air walker boot for several weeks which will allow the tendon to rest and heal, especially if a posterior tibial tendon tear is noted on MRI.
Causes Damage to the posterior tendon from overuse is the most common cause for adult acquired flatfoot. Running, walking, hiking, and climbing stairs are activities that add stress to this tendon, and this overuse can lead to damage. Obesity, previous ankle surgery or trauma, diabetes (Charcot foot), and rheumatoid arthritis are other common risk factors. Symptoms Patients often experience pain and/or deformity at the ankle or hindfoot. When the posterior tibial tendon does not work properly, a number of changes can occur to the foot and ankle. In the earlier stages, symptoms often include pain and tenderness along the posterior tibial tendon behind the inside of the ankle. As the tendon progressively fails, deformity of the foot and ankle may occur. This deformity can include progressive flattening of the arch, shifting of the heel so that it no longer is aligned underneath the rest of the leg, rotation and deformity of the forefoot, tightening of the heel cord, development of arthritis, and deformity of the ankle joint. At certain stages of this disorder, pain may shift from the inside to the outside aspect of the ankle as the heel shifts outward and structures are pinched laterally. Diagnosis Perform a structural assessment of the foot and ankle. Check the ankle for alignment and position. When it comes to patients with severe PTTD, the deltoid has failed, causing an instability of the ankle and possible valgus of the ankle. This is a rare and difficult problem to address. However, if one misses it, it can lead to dire consequences and potential surgical failure. Check the heel alignment and position of the heel both loaded and during varus/valgus stress. Compare range of motion of the heel to the normal contralateral limb. Check alignment of the midtarsal joint for collapse and lateral deviation. Noting the level of lateral deviation in comparison to the contralateral limb is critical for surgical planning. Check midfoot alignment of the naviculocuneiform joints and metatarsocuneiform joints both for sag and hypermobility. Non surgical Treatment Flatfoot deformity can be treated conservatively or with surgical intervention depending on the severity of the condition. When people notice their arches flattening, they should immediately avoid non-supportive shoes such as flip-flops, sandals or thin-soled tennis shoes. Theses shoes will only worsen the flatfoot deformity and exacerbate arch pain. Next, custom orthotics are essential for people with collapsed arches. Over-the-counter insoles only provide cushion and padding to the arch, whereas custom orthotics are fabricated to specifically fit the patient?s foot and provide support in the arch where the posterior tibial tendon is unable to anymore. Use of custom orthotics in the early phases of flatfoot or PTTD can prevent worsening of symptoms and prevent further attenuation or injury to the posterior tibial tendon. In more severe cases of flatfoot deformity an ankle foot orthosis (AFO) such as a Ritchie brace is needed. This brace provides more support to the arch and hindfoot rather than an orthotic but can be bulky in normal shoegear. Additional treatment along with use of custom orthotics is use of non-steroidal anti-inflammatories (NSAIDS) such as Advil, Motrin, or Ibuprofen which can decrease inflammation to the posterior tibial tendon. If pain is severe, the patient may need to be placed in a below the knee air walker boot for several weeks which will allow the tendon to rest and heal, especially if a posterior tibial tendon tear is noted on MRI. 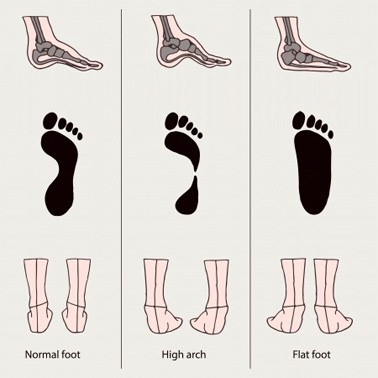 Surgical Treatment For more chronic flatfoot pain, surgical intervention may be the best option. Barring other serious medical ailments, surgery is a good alternative for patients with a serious problem. There are two surgical options depending on a person?s physical condition, age and lifestyle. The first type of surgery involves repair of the PTT by transferring of a nearby tendon to help re-establish an arch and straighten out the foot. After this surgery, patients wear a non-weight bearing support boot for four to six weeks. The other surgery involves fusing of two or three bones in the hind foot below the ankle. While providing significant pain relief, this option does take away some hind foot side-to-side motion. Following surgery, patients are in a cast for three months. Surgery is an effective treatment to address adult-acquired flatfoot, but it can sometimes be avoided if foot issues are resolved early. That is why it is so important to seek help right away if you are feeling ankle pain. But perhaps the best way to keep from becoming flatfooted is to avoid the risk factors altogether. This means keeping your blood pressure, weight and diabetes in check.
Surgical Treatment For more chronic flatfoot pain, surgical intervention may be the best option. Barring other serious medical ailments, surgery is a good alternative for patients with a serious problem. There are two surgical options depending on a person?s physical condition, age and lifestyle. The first type of surgery involves repair of the PTT by transferring of a nearby tendon to help re-establish an arch and straighten out the foot. After this surgery, patients wear a non-weight bearing support boot for four to six weeks. The other surgery involves fusing of two or three bones in the hind foot below the ankle. While providing significant pain relief, this option does take away some hind foot side-to-side motion. Following surgery, patients are in a cast for three months. Surgery is an effective treatment to address adult-acquired flatfoot, but it can sometimes be avoided if foot issues are resolved early. That is why it is so important to seek help right away if you are feeling ankle pain. But perhaps the best way to keep from becoming flatfooted is to avoid the risk factors altogether. This means keeping your blood pressure, weight and diabetes in check.